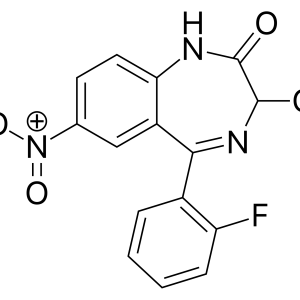
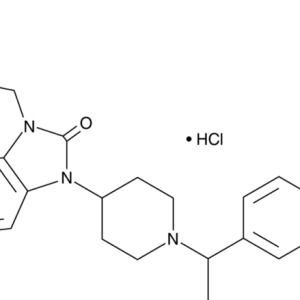
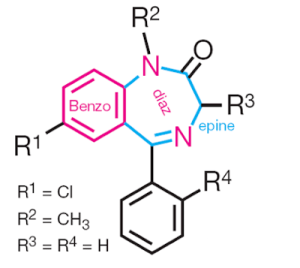
The term “benzodiazepines” reflects the chemical affiliation to drugs with a 5-aryl-1,4-benzodiazepine structure, which appeared as a result of combining a benzene ring into a seven-membered diazepine ring. Various benzodiazepines are widely used in medicine. Three drugs have been well studied and are most widely used for the needs of anesthesiology in all countries: midazolam, diazepam and lorazepam.
Benzodiazepines
Benzodiazepines: a place in therapy
In clinical anesthesiology and intensive care, benzodiazepines are used for premedication, induction of anesthesia, its maintenance, for sedation during interventions under regional and local anesthesia, during various diagnostic procedures (for example, endoscopy, endovascular surgery), sedation in the NICU.
Barbiturates and antipsychotics have been virtually eliminated from use as a component of premedication by benzodiazepines due to fewer adverse events. For this purpose, medications are prescribed orally or intravenously. Midazolam is distinguished by the possibility of its administration rectally (an advantage in children); in addition, not only its tablet form, but also an injectable solution can be administered orally. The anxiolytic and sedative effects are most pronounced and occur faster when using midazolam. The development of lorazepam effects is slower. It should be noted that 10 mg of diazepam is equivalent to 1-2 mg of lorazepam or 3-5 mg of midazolam.
Benzodiazepines have been widely used to provide conscious sedation during regional and local anesthesia. Moreover, their particularly desirable properties are anxiolysis, amnesia and an increase in the seizure threshold for local anesthetics. Benzodiazepines should be administered by titration until adequate sedation or dysarthria is achieved. This is achieved by administering a loading dose followed by repeated bolus injections or prolonged infusion. There is not always a correlation between the level of sedation and amnesia (the appearance of wakefulness and lack of memory of it) caused by all benzodiazepines. But the duration of amnesia is especially unpredictable when using lorazepam.
In general, among other sedative-hypnotic drugs, benzodiazepines provide the best degree of sedation and amnesia.
In the NICU, benzodiazepines are used to provide conscious sedation, as well as deep sedation to synchronize the patient’s breathing with the operation of the respirator in the NICU. In addition, benzodiazepines are used to prevent and relieve seizures and delirious states.
The rapid development of the effect and the absence of venous complications make midazolam preferable to other benzodiazepines for the induction of general anesthesia. However, in terms of sleep onset, midazolam is inferior to hypnotics from other groups, such as sodium thiopental and propofol. The rate of action of benzodiazepines is influenced by the dose used, the rate of administration, the quality of premedication, age and general physical status, as well as combination with other medications. Usually, the induction dose is reduced by 20% or more in patients over 55 years of age and patients at high risk of complications (ASA Class III (American Association of Anesthesiologists) and higher). By a rational combination of two or more anesthetics (coinduction), a reduction in the amount of each drug administered is achieved. With short-term interventions, the introduction of induction doses of benzodiazepines is not fully justified, since this lengthens the wake-up time.
Benzodiazepines are able to protect the brain from hypoxia in some cases and are used in critical conditions. Midazolam demonstrates the greatest effectiveness in this case, although it is inferior to that of barbiturates.
The benzodiazenine receptor antagonist flumazenil is used in the practice of anesthesiology for therapeutic purposes – to eliminate the effects of benzodiazepine receptor agonists after surgical interventions and diagnostic procedures. At the same time, it actively eliminates sleep, sedation and respiratory depression rather than amnesia. Drugs should be administered intravenously by titration until the desired effect is achieved. It is important to keep in mind that higher doses will be required for stronger benzodiazepines. In addition, repeated doses or infusion of flumazenil may be required for long-acting benzodiazepines due to the likelihood of relapse. The use of flumazenil to neutralize the effects of BD does not provide grounds for allowing patients to drive a vehicle.
Another use of flumazenil is diagnostic. It is administered for the differential diagnosis of possible benzodiazepine poisoning. At the same time, if there is no decrease in the degree of sedation, other causes of CNS depression are most likely.
During prolonged sedation with benzodiazepines, flumazenil can be used to create a “diagnostic window”.
Mechanism of action and pharmacological effects
Benzodiazepines have many properties that are desirable for anesthesiologists. At the level of the central nervous system, they have various pharmacological effects, of which sedative, anxiolytic (anxiety reduction), hypnotic, anticonvulsant, muscle relaxant and amnesic (anterograde amnesia) are fundamentally important.
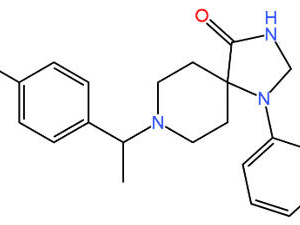
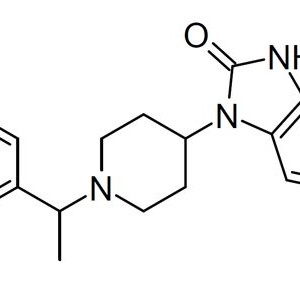
Benzodiazepines exhibit all their pharmacological effects by facilitating the action of GABA, the main inhibitory neurotransmitter in the central nervous system, which balances the effect of activating neurotransmitters. The discovery of the benzodiazepine receptor in the 1970s largely explained the mechanism of action of benzodiazepines on the central nervous system. One of the two GABA receptors, the GABA-receptor pentameter complex, is a large macromolecule and contains protein units (alpha, beta, and gamma) that include various ligand binding sites for GABA, benzodiazepines, barbiturates, and alcohol. Several different subunits of the same type (six different a, four beta, and three gamma) with different abilities to form a chloride channel were found. The structure of receptors in different parts of the central nervous system may be different (for example, alpha1, beta and gamma2 or alpha3, beta1 and gamma2), which determines different pharmacological properties. For affinity to DB, the receptor must have a y2 subunit. There is a definite structural correspondence between the GABAA receptor and the nicotinic acetylcholine receptor.
By binding to specific sites of the GABAA receptor complex located on the subsynaptic membrane of the effector neuron, benzodiazepines strengthen the binding of the receptor to GABAA, which enhances the opening of channels for chlorine ions. Increased penetration of chlorine ions into the cell leads to hyperpolarization of the postsynaptic membrane and resistance of neurons to excitation. Unlike barbiturates, which increase the duration of the opening of ion channels, benzodiazepines increase the frequency of their opening.
The effect of benzodiazepines largely depends on the dose of the drug used. The order of occurrence of the central effects is as follows: anticonvulsant effect, anxiolytic effect, mild sedation, decreased concentration, intellectual inhibition, amnesia, deep sedation, relaxation, sleep. It is assumed that binding of the benzodiazepine receptor by 20% provides anxiolysis, capture of 30-50% of the receptor is accompanied by sedation, and stimulation of > 60% of the receptor is required to turn off consciousness. It is possible that the difference in the effects of benzodiazepines on the central nervous system is due to the effects on different subtypes of receptors and/or on different numbers of occupied receptors.
It is also possible that the anxiolytic, anticonvulsant, and muscle relaxant effects are realized through the GABAA receptor, and the hypnotic effect is mediated by changing the flow of calcium ions through potential-dependent channels. Sleep is close to physiological with characteristic EEG phases.
The highest density of benzodiazepine receptors is found in the cerebral cortex, hypothalamus, cerebellum, hippocampus, olfactory bulb, substantia nigra, and inferior tubercle; lower density is found in the striatum, lower brainstem, and spinal cord. The degree of GABAA receptor modulation is limited (the so-called “limiting effect” of benzodiazepines on central nervous system depression), which determines the rather high safety of DB use. The predominant localization of GABAA receptors in the central nervous system determines the minimal effects of drugs outside of it (minimal circulatory effects).
There are 3 types of ligands acting on the benzodiazepine receptor: agonists, antagonists and inverted agonists. The action of agonists (e.g. diazepam) is described above. Agonists and antagonists bind the same (or overlapping) sites of the receptor, forming various reversible connections with it. Antagonists (for example, flumazenil) occupy the receptor, but do not have their own activity and therefore block the action of both agonists and inverted agonists. Inverted agonists (for example, beta-carbolines) reduce the inhibitory effect of GABA, which leads to anxiety and seizures. There are also endogenous agonists with benzodiazepine-like properties.
Benzodiazepines vary in effectiveness with respect to each pharmacological action, depending on affinity, stereospecificity, and intensity of binding to the receptor. The strength of the ligand is determined by its affinity with the benzodiazepine receptor, and the duration of the effect is determined by the rate of drug removal from the receptor According to the strength of its hypnotic effect, benzodiazepines are arranged in the following order, lorazepam > midazolam > flunitrazepam > diazepam.
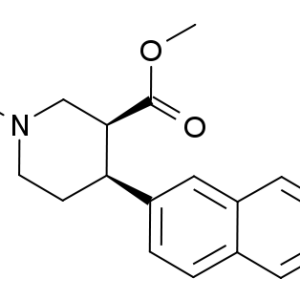
Unlike all other sedative-hypnotic drugs, most benzodiazepines have a specific receptor antagonist, flumazenil. It belongs to the group of imidobenzodiazepines. While structurally similar to the main benzodiazepines, the phenyl group of flumazenyl is replaced by a carbonyl group.
As a competitive antagonist, flumazenil does not displace the agonist from the receptor, but occupies the receptor at the moment of separation of the agonist from it. Due to the fact that the binding period of the ligand to the receptor lasts up to several seconds, the binding of the receptor to the agonist or antagonist is dynamically updated. The receptor occupies the ligand that has a greater affinity for the receptor and whose concentration is higher. The affinity of flumazenil for the benzodiazepine receptor is extremely high and exceeds that for agonists, especially diazepam. The concentration of the drug in the receptor area is determined by the dose used and the rate of its elimination.

Benzodiazepines
Effects on cerebral blood flow
The degree of decrease in MC, metabolic pmoA and decrease in intracranial pressure depend on the dose of benzodiazepine and are inferior to those for barbiturates. Despite a slight increase in RaSO2, benzodiazepines in induction doses cause a decrease in MC, but the ratio of MC and PMO2 does not change.
Electroencephalographic picture
The electroencephalographic picture during benzodiazepine anesthesia is characterized by the appearance of rhythmic beta activity. There is no tolerance to the effects of benzodiazepines on the EEG. Unlike barbiturates and propofol, midazolam does not induce an isoelectric EEG.
With the introduction of DB, the amplitude of cortical SSR decreases, the latency of the early potential shortens and the peak latency lengthens. Midazolam also reduces the amplitude of the peaks of the mid-latency SVPs of the brain. Other criteria for the depth of benzodiazepine anesthesia can be the registration of BIS and the AAI™ ARX index (an improved version of SVP treatment).
Benzodiazepines rarely cause nausea and vomiting. The antiemetic effect attributed to them by some authors is small and is rather due to the effect of sedation.
Effects on the cardiovascular system
With isolated use, benzodiazepines have a moderate effect on the cardiovascular system. In both healthy subjects and patients with heart disease, the predominant changes in hemodynamics are a slight decrease in blood pressure due to a decrease in heart rate. Heart rate, SV, and ventricular filling pressure change to a lesser extent.
In addition, when the equilibrium concentration of the drug in the plasma is reached, there is no further decrease in blood pressure. It is assumed that such a relatively mild effect on hemodynamics is associated with the preservation of protective reflex mechanisms, although the baroreflex is changing. The effect on blood pressure depends on the dose of the drug and is most pronounced in midazolam. But at the same time, even in high doses and in cardiac surgery patients, hypotension is not excessive. By reducing pre- and post-loading in patients with congestive heart failure, benzodiazepines may even increase SV.
The situation changes when benzodiazepines are combined with opioids. In this case, the decrease in blood pressure is more significant than for each drug, due to the pronounced additive effect. It is possible that this synergy is due to a decrease in the tone of the sympathetic nervous system. A more significant hemodynamic depression is observed in patients with hypovolemia.
Benzodiazepines have minor analgesic properties and do not prevent reactions to traumatic manipulations, in particular to tracheal intubation. The additional use of opioids is most justified at such stages.
Effects on the respiratory system
Benzodiazepines have a central effect on respiration and, like most intravenous anesthetics, increase the threshold level of carbon dioxide to stimulate the respiratory center. The result is a decrease in respiratory volume (UP to) and minute respiratory volume (MOD). The rate of respiratory depression and its severity are higher in midazolam. In addition, faster administration of the drug leads to a faster development of respiratory depression. Respiratory depression is more pronounced and lasts longer in patients with COPD. Lorazepam is less respiratory depressant than midazolam and diazepam, but in combination with opioids, all benzodiazepines have a synergistic suppressive effect on the respiratory system. Benzodiazepines suppress the swallowing reflex and reflex activity of the upper respiratory tract. Like other hypnotics, benzodiazepines can cause respiratory arrest. The likelihood of apnea depends on the dose of benzodiazepine used and the combination with other medications (opioids). In addition, the frequency and severity of respiratory depression increase in debilitating diseases and in senile patients. There is evidence of a slight synergistic effect on respiration of midazolam and local anesthetics administered subarachnoid.
Effects on the gastrointestinal tract
Benzodiazepines do not have an adverse effect on the gastrointestinal tract, including when ingested and rectally administered (midazolam). They do not induce liver enzymes.
There is evidence of a decrease in nocturnal secretion of gastric juice and a slowdown in intestinal motility while taking diazepam and midazolam, but these manifestations are likely with prolonged use of the drug. In rare cases, nausea, vomiting, hiccups, and dry mouth may occur when taking benzodiazepine orally.
Effects on the endocrine response
There is evidence that benzodiazepines reduce the level of catecholamines (cortisol). This property is not the same for all benzodiazepines. It is believed that the increased ability of alprazolam to suppress the secretion of adrenocorticotropic hormone (ACTH) and cortisol contributes to its pronounced effectiveness in the treatment of depressive syndromes.
Effects on neuromuscular transmission
Benzodiazepines do not have a direct effect on neuromuscular transmission. Their muscle relaxant effect is carried out at the level of the insertion neurons of the spinal cord, and not at the periphery. However, the severity of muscle relaxation caused by benzodiazepines is insufficient to perform surgical interventions. Benzodiazepines do not determine the mode of administration of relaxants, although they may potentiate their effect to some extent. In animal experiments, high doses of benzodiazepine inhibited the conduction of impulses along the neuromuscular junction.
Other effects
Benzodiazepines increase the primary seizure threshold (important when using local anesthetics) and are able to protect the brain from hypoxia to some extent.
Tolerance
Prolonged administration of benzodiazepines causes a decrease in their effectiveness. The mechanism of tolerance development is not fully understood, but it is assumed that prolonged exposure to benzodiazepines is the cause of decreased binding to the GABAA receptor. This explains the need to use high doses of benzodiazepines for anesthesia in patients who have been taking them for a long time.
Marked tolerance to benzodiazepines is typical for drug addicts. It can be expected to appear in patients with burns who undergo frequent bandages under anesthesia. In general, tolerance to benzodiazepines is less likely than to barbiturates.
Pharmacokinetics
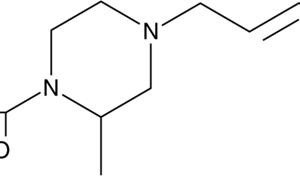
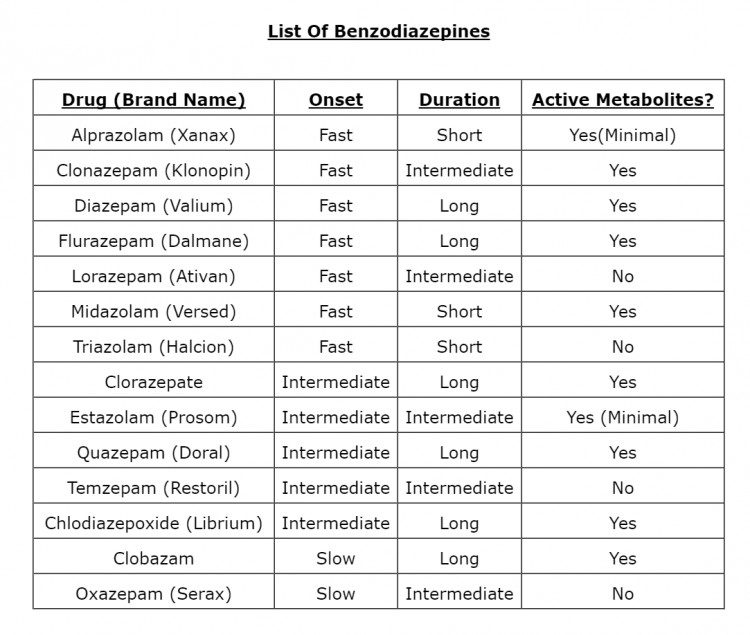
According to the duration of elimination from the body, benzodiazepines are divided into 3 groups. Medications with a prolonged T1/2 (> 24 hours) include chlordiazepoxide, diazepam, medazepam, nitrazepam, phenazepam, flurazepam, alprazolam. Oxazepam, lorazepam, and flunitrazepam have an average elimination duration (T1/2 (3 from 5 to 24 hours). Midazolam, triazolam and temazepam have the shortest T1/2 (< 5 h).
Benzodiazepines
Benzodiazepines can be administered orally, rectally, intramuscularly or intravenously.
All benzodiazepines are fat-soluble compounds. When ingested in tablet forms, they are well and completely absorbed, mainly in the duodenum. Their bioavailability is 70-90%. Midazolam in the form of an injectable solution is well absorbed from the gastrointestinal tract when taken orally, which is important in children’s practice. Midazolam is rapidly absorbed by rectal administration and reaches its maximum plasma concentration within 30 minutes. Its bioavailability with this route of administration is approaching 50%.
With the exception of lorazepam and midazolam, the absorption of benzodiazepines from muscle tissue is incomplete and uneven and, due to the need to use a solvent, is associated with the development of local reactions with intramuscular administration.
In the practice of anesthesiology and intensive care, the intravenous route of administration of benzodiazepine is preferred. Diazepam and lorazepam are insoluble in water. Propylene glycol is used as a solvent, which is responsible for local reactions when the drug is administered. The imidazole ring of midazolam gives it stability in solution, rapid metabolism, the highest fat solubility, as well as solubility in water at low pH. Midazolam is specially prepared in an acid buffer with a pH of 3.5, because The opening of the imidazole ring depends on pH: at pH < 4, the ring is open and the drug is water-soluble, at pH > 4 (physiological values), the ring closes and the drug becomes fat-soluble. The water solubility of midazolam does not require the use of an organic solvent, which causes pain during intravenous administration and prevents absorption during intramuscular injection. In the systemic circulation, benzodiazepines, with the exception of flumazenil, are strongly bound to plasma proteins (80-99%). Benzodiazepine molecules are relatively small and have high fat solubility at physiological pH. This explains the rather high volume of distribution and their rapid effect on the central nervous system. The maximum concentrations of the drug (Cmax) in the systemic bloodstream are reached after 1-2 hours. Due to the greater solubility in fats during intravenous administration, midazolam and diazepam have a faster onset of action than lorazepam. However, the rate of midazolam equilibrium concentration in the effector zone of the brain is significantly lower than that of sodium thiopental and propofol. The onset and duration of a single bolus dose of benzodiazepine depend on their fat solubility.
Like the onset of action, the duration of the effect is also related to the fat solubility and plasma concentration of the drug. The binding of benzodiazepine to plasma proteins is parallel to their fat solubility, i.e. high fat solubility increases protein binding. The high degree of protein binding limits the effectiveness of hemodialysis in cases of diazepam overdose.
Prolonged T1/2 in the elimination phase of diazepam is explained by its large volume of distribution and slow extraction in the liver. The shorter T1/2 beta of lorazepam compared to diazepam is due to its lower fat solubility and lower volume of distribution. Despite its high fat solubility and high volume of distribution, midazolam has the shortest T1/2 beta because it is extracted by the liver at a faster rate than other benzodiazepines.
T1/2 of benzodiazepine in children (except infants) is somewhat shorter. In the elderly and patients with impaired liver function (including congestive nature), T1/2 may increase significantly. The increase in T1/2 is especially significant (up to 6 times even for midazolam) at high steady-state concentrations of benzodiazepine created by continuous infusion for sedation. The volume of distribution is increased in obese patients.
At the beginning of IC, the concentration of benzodiazepine in plasma decreases, and after the end it increases. Such changes are associated with a redistribution of the composition of the fluid from the apparatus to the tissues, a change in the proportion of the non-protein fraction of the drug. As a result, T1/2 of benzodiazepine is prolonged after the procedure.
The elimination of benzodiazepines largely depends on the rate of biotransformation that occurs in the liver. Benzodiazepines are metabolized in two main ways: by microsomal oxidation (N-dealkylation, or aliphatic hydroxylation) or by binding (conjugation) to form more water-soluble glucuronides. The predominance of one of the biotransformation pathways is clinically important, since oxidative processes can change under the influence of external factors (for example, age, liver disease, and other drugs), and conjugation is less dependent on these factors.
Due to the presence of the imidazole ring, midazolam oxidizes faster than others and has a more significant hepatic clearance compared to diazepam. Age decreases, and smoking increases the hepatic clearance of diazepam. For midazolam, these factors are not significant, but its clearance increases with alcohol abuse. Inhibition of the function of oxidative enzymes (for example, cimetidine) reduces the clearance of diazepam, but does not affect the conversion of lorazepam. The hepatic clearance of midazolam is 5 times higher than that of lorazepam and 10 times higher than that of diazepam. The hepatic clearance of midazolam is inhibited by fentanyl, as its metabolism is also associated with the participation of cytochrome P450 isoenzymes. It should be borne in mind that the enzyme activity is influenced by many factors, including hypoxia, inflammatory mediators, therefore, the elimination of midazolam in ICU patients becomes poorly predictable. There is also evidence of genetic racial characteristics of benzodiazepine metabolism, in particular, a decrease in hepatic clearance of diazepam in Asians.
Benzodiazepine metabolites have different pharmacological activity and can cause a long-lasting effect with prolonged use. Lorazepam forms five metabolites, of which only the main one binds to glucuronide, is not metabolically active and is rapidly excreted in the urine. Diazepam has three active metabolites: desmethyldiazepam, oxazepam and temazepam. Desmethyldiazepam is metabolized significantly longer than oxazepam and temazepam and is only slightly inferior to the strength of diazepam. Its T1/2 is 80-100 hours, so it determines the total duration of action of diazepam. When ingested, up to 90% of diazepam is excreted by the kidneys as glucuronides, up to 10% in the faeces, and only about 2% is excreted unchanged in the urine. Flunitrazepam is oxidized to three active metabolites, the main of which is demethylflunitrazepam. The main metabolite of midazolam, alpha-hydroxymethylmidazolam (alpha-hydroxymidazolam), has 20-30% precursor activity. It quickly conjugates and is excreted in the urine by 60-80% within a day. The other two metabolites are found in insignificant amounts. In patients with normal kidney and liver function, the value of midazolam metabolites is low.
Due to the fact that the change in the concentration of benzodiazepines in the blood does not correspond to the kinetics of the first order, with the infusion method of their administration, it is necessary to follow the context-sensitive T1/2. It is clear from the figure that the accumulation of diazepam is such that after a short infusion, T1/2 increases several times. The time of cessation of the effect can be approximately predicted only with midazolam infusion.
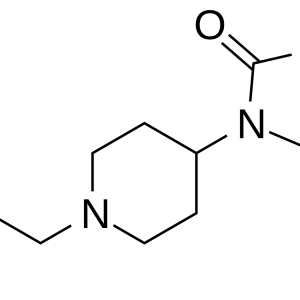
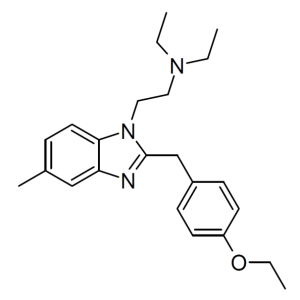
Recently, the possibilities of clinical use of two benzodiazepine receptor agonists, RO 48-6791 and RO 48-8684, which have a high volume of distribution and clearance compared to midazolam, have been studied. Therefore, recovery after anesthesia is faster (about 2 times). The appearance of such drugs will bring benzodiazepines closer to propofol in terms of the rate of development and termination of action. In the longer term, the creation of benzodiazepines, rapidly metabolized by blood esterases.
A specific antagonist of benzodiazepine receptors, flumazenil is able to dissolve in both fats and water, which allows it to be released as an aqueous solution. It is possible that the relatively low binding to plasma proteins contributes to the rapid onset of action of flumazenil. Flumazenil has the shortest T1/2 and the highest clearance. This feature of pharmacokinetics explains the possibility of reseditation at a relatively high dose of the administered agonist with a large T1/2- T1/2 is more variable in children over 1 year old (from 20 to 75 minutes), but generally shorter than in adults.
Flumazenil is almost entirely metabolized in the liver. The details of metabolism are still poorly understood. It is believed that the metabolites of flumazenil (N-desmethylflumazenyl, N-desmethiflumazenylic acid and flumazenylic acid) form the corresponding glucuronides, which are excreted in the urine. There is also evidence of the final metabolism of flumazenil to pharmacologically neutral carbonic acid. The total clearance of flumazenil approaches the rate of hepatic blood flow. Its metabolism and elimination are slowed down in patients with impaired liver function. Agonists and antagonists of benzodiazepine receptors do not affect the pharmacokinetics of each other.
Benzodiazepine addiction and withdrawal syndrome
Benzodiazepines, even in therapeutic doses, can cause dependence, which is confirmed by the appearance of physical and psychological symptoms after dose reduction or drug withdrawal. Symptoms of addiction may develop after 6 months or more of using commonly prescribed mild benzodiazepines. The severity of dependence and withdrawal symptoms is significantly lower than that of other psychotropic drugs (for example, opioids and barbiturates).
Withdrawal symptoms are usually manifested by irritability, insomnia, tremor, loss of appetite, sweating, and confusion. The timing of the development of withdrawal syndrome corresponds to the duration of T1/2 medications. Withdrawal symptoms usually appear within 1-2 days for short-acting medications and within 2-5 days (sometimes up to several weeks) for long-acting medications. In patients with epilepsy, abrupt withdrawal of benzodiazepine can lead to seizures.
Pharmacological effects of flumazenil
Flumazenil has weak pharmacological effects on the central nervous system. It does not affect the EEG and metabolism in the brain. The order of elimination of the effects of benzodiazepine is the reverse of the order of their occurrence. The hypnotic and sedative effects of benzodiazepine after intravenous administration are eliminated quickly (within 1-2 minutes).
Flumazenil does not cause respiratory depression, does not affect blood circulation even in high doses and in patients with coronary artery disease. It is extremely important that it does not cause hyperdynamics (as, for example, naloxone) and does not increase the level of catecholamines. Its effect on benzodiazepine receptors is selective, so it does not eliminate opioid-induced analgesia and respiratory depression, does not alter the effects of volatile anesthetics, and does not affect the effects of barbiturates and ethanol.
Contraindications to the use of benzodiazepines
Contraindications to the use of benzodiazepines are individual intolerance or hypersensitivity to the components of the dosage form, in particular to propylene glycol. In anesthesiology, most contraindications are relative. These include myasthenia gravis, severe hepatic and renal insufficiency, first trimester of pregnancy, breast-feeding, and angle-closure glaucoma.
A contraindication to the appointment of a benzadiazenine receptor antagonist is hypersensitivity to flumazenil. Although there is no convincing evidence of withdrawal reactions during its administration, flumazenil is not recommended for use in situations where benzodiazepines are used for potentially life-threatening conditions (for example, epilepsy, intracranial hypertension, traumatic brain injury). It should be used cautiously in cases of mixed overdose of the drug, when benzodiazepines “cover up” the toxic effect of other drugs (for example, cyclic antidepressants).
The factor significantly limiting the use of flumazenil is its high cost. The availability of the drug may increase the frequency of use of benzodiazepines, although it will not affect their safety.
Tolerance and side effects
In general, benzodiazepines are relatively safe drugs, for example, compared to barbiturates. Midazolam has the best tolerance.
The spectrum and severity of side effects of benzodiazepines depends on the purpose, duration of use and methods of administration. With constant intake, drowsiness and fatigue are typical. When benzodiazepines are used for sedation, induction, or maintenance of anesthesia, they can cause respiratory depression, severe and prolonged postoperative amnesia, and sedation. These residual effects can be eliminated with flumazenil. Respiratory depression is eliminated by respiratory support and/or administration of flumazenil. Circulatory depression rarely requires specific measures.
Significant side effects of diazepam and lorazepam are irritation of the veins and delayed thrombophlebitis, which is associated with poor water solubility of the drug and the use of solvents. For the same reason, water-insoluble benzodiazepines should not be injected into the artery. According to the severity of the local irritant effect of benzodiazepines, they are arranged in the following order:
Diazepam > lorazepam > flunitrazepam > midazolam. It is possible to reduce the severity of this side effect by diluting the drug sufficiently, injecting the drug into large veins, or reducing the rate of administration of the drug. The introduction of diazepam into the dosage form as a solvent of the fat emulsion also reduces its irritating effect. Accidental intraarterial administration (in particular, flunitrazepam) can lead to necrosis.
An important advantage of using benzodiazepines (especially midazolam) is the low probability of allergic reactions.
In rare cases, paradoxical reactions (agitation, excessive activity, aggressiveness, convulsive readiness, hallucinations, insomnia) are possible when using benzodiazepines.
Benzodiazepines do not have embryotoxic, teratogenic or mutagenic effects. All other toxic effects are associated with overdose.
The safety of flumazenil exceeds that of the DRUG agonists. It is well tolerated by all age groups of patients and has no local irritant effect. In doses 10 times higher than recommended for clinical use, it does not cause an agonistic effect. Flumazenil does not cause toxic reactions in animals, although the effect on the human fetus has not been established.
Interaction
Benzodiazepines interact with various groups of drugs that are used both to provide surgery and to treat underlying and concomitant diseases.
Favorable combinations
The combined use of benzodiazepines and other drugs for anesthesia is beneficial in many ways, because their synergy allows you to reduce the amount of each drug individually, and therefore reduce their side effects. In addition, it is possible to significantly save expensive drugs without compromising the quality of anesthesia.
Often, the use of diazepam for premedication does not provide the desired effect. Therefore, it is advisable to combine it with other medicines. The quality of premedication largely determines the amount of induction agents administered, and hence the likelihood of side effects.
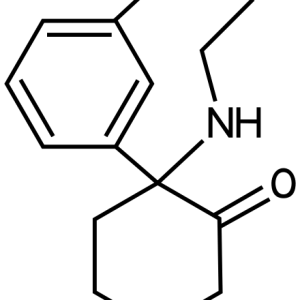
Benzodiazepines reduce the need for opioids, barbiturates, propofol. They neutralize the adverse effects of ketamine (psychomimetic), gamma-hydroxybutyric acid (GHB) and etomidate (myoclonia). All this serves as the basis for the use of rational combinations of these drugs for conducting the procedure. At the stage of maintaining anesthesia, such combinations provide greater stability of anesthesia and also reduce the time of awakening. Midazolam reduces the effect of volatile anesthetics (in particular, halothane by 30%).