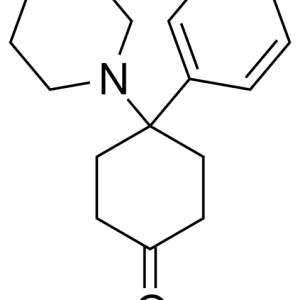
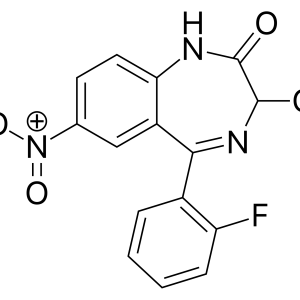
Benzodiazepine derivatives, anxiety–relieving anxiolytics, are called tranquilizers in the old way. Drugs of this group enhance the effects of GABA (gamma-amino-butyric acid), the main inhibitory mediator in the central nervous system. They have a weak effect on serotonin and dopamine receptors. The effects are due to the influence on various parts of the central nervous system: the reticular formation of the brainstem and the nonspecific nuclei of the thalamus (sedative effect), the amygdala complexes of the limbic system (anxiolytic), the polysynapses of the spinal cord (muscle relaxant) and the hippocampus (anticonvulsant). Sedation caused by benzodiazepines is manifested by suppression of the reaction to constant stimuli with a decrease in the level of thinking and activity. They are characterized by anterograde amnesia, when it is impossible to recall what happened during the action of the drug. At the same time, contact with the patient remains. This complication, by the way, can be very convenient for unpleasant medical manipulations, including chemotherapy. Drugs of this group are anesthetics and, in combination with other drugs, can be used in palliative oncology precisely as painkillers.
The presence of very beneficial properties has caused the excessive use of these drugs, which leads to psychological and physical dependence. In the early 90s, benzodiazepines were ranked 18th to 20th among the most consumed drugs in the United States. In Russia, all drugs in this group are under the supervision of the Drug Control Committee, as they are highly addictive drugs. This does not make them unavailable, it’s just that there are restrictions in the number and frequency of discharge. They are absolutely indispensable for the prevention of pre-nausea and vomiting.
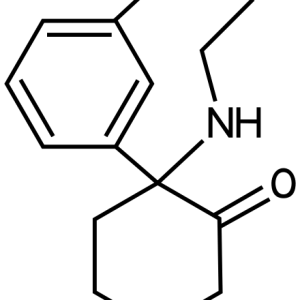
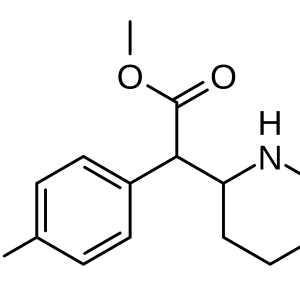
Diazepam (sibazone, seduxene, relanium) may be useful for relieving delayed vomiting, as it has an injectable form. Diazepam is more lipophilic than lorazepam, so the effects of the latter on the central nervous system are delayed. The rate of metabolic transformation and elimination is too low, so the main effects are prolonged. The half–life of lorazepam is from 10 to 18 hours, diazepam – 48-150 hours, phenozepam – up to 18 hours.
Long elimination half-lives can lead to undesirable excessive inhibition of the central nervous system and are caused by the formation of active forms of metabolites. The half-life of diazepam increases with age, but its elimination from the body remains constant. On the other hand, the shorter the half-life, the more severe the withdrawal syndrome characteristic of tranquilizers, since trace concentrations of the drug persist in plasma for a long time. The “withdrawal” syndrome strongly resembles an alcoholic hangover. Drugs in this group are characterized by a pronounced cross-dependence, when withdrawal symptoms caused by, for example, lorazepam can be stopped by taking diazepam or phenozepam, and vice versa. Classical physical dependence, however, develops very rarely, only with prolonged use of very high doses, for diazepam it is 8-10 tablets per day for more than 2-3 months. For most sleeping pills (except benzodiazepines), a dose 10 times higher than the sleeping pill can be fatal. There is an antidote for benzodiazepines, flumazenil. But the main disadvantage of benzodiazepines is the increased depression of the central nervous system when taken together with other sedatives or alcohol.