Composition
Active ingredient: methadone;
1 tablet contains methadone hydrochloride 5 mg, 10 mg, 25 mg or 40 mg;
excipients: lactose monohydrate, microcrystalline cellulose, corn starch, magnesium stearate.
Dosage form
Pills.
Basic physical and chemical properties:
tablets of 5 mg and 10 mg are white or almost white in color, round cylindrical shape with a flat surface and chamfers;
tablets 25 mg: white or almost white in color, round cylindrical shape with a flat surface, chamfers and a risk on one side;
tablets 40 mg: white or almost white in color, round cylindrical shape with convex surfaces, chamfers and a risk on one side.
Pharmacotherapeutic group
Drugs used for opiate addiction.
Pharmacological properties
Pharmacodynamics.
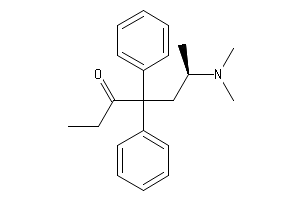
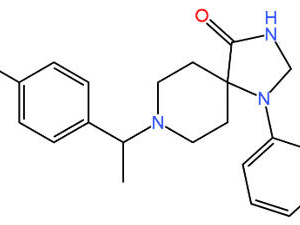
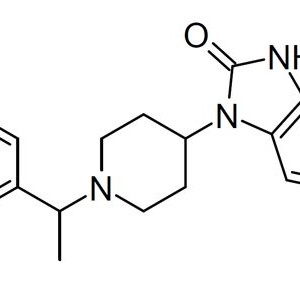
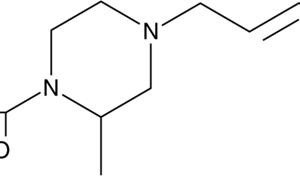
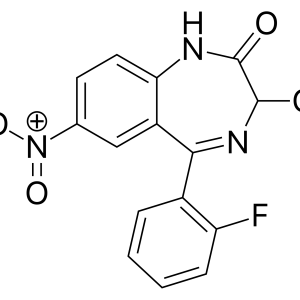
Methadone is a synthetic derivative of diphenylheptan and differs significantly in chemical structure from morphine and heroin. However, the main pharmacological properties of these drugs are similar: they cause depression of the respiratory center, increased tone of smooth muscles, constipation and other symptoms characteristic of the action of opioids.
Methadone has specific properties of a partial agonist of the m- and k-receptors of the opioidergic system of the brain. The analgesic activity of the drug is realized by inhibiting the interneuronal transmission of pain impulses at the spinal and supraspinal levels of the central nervous system (CNS). In addition to analgesia, methadone can cause pronounced psychotropic effects, in particular, a feeling of euphoria and supra-real mental comfort.
The specific pharmacotherapeutic effects of methadone are based on two main mechanisms. First, methadone, as an agonist of opiate receptors, inhibits the clinical manifestations of withdrawal symptoms in patients with opioid addiction. Secondly, prolonged use of methadone can lead to the development of cross-tolerance, which will lead to a decrease in the severity of specific psychotropic effects in patients dependent on injectable drugs (heroin, morphine and others).
The effect of methadone begins 30-60 minutes after ingestion and quickly reaches its maximum. The duration of action of the drug is on average 6-8 hours, but in patients with physical dependence on opioids it can increase to 22-48 hours.
Repeated use of the drug leads to cumulative effects and the development of prolonged sedation.
Pharmacokinetics.
The degree of absorption of methadone with oral administration reaches 92%. The drug is rapidly distributed in the tissues of the body. Metabolism occurs in the liver, where methadone is subject to N-demethylation. Methadone and its metabolites are excreted from the body by the kidneys or biliary tract. When doses exceeding 160 mg per day are used, renal elimination becomes the main route of elimination, while up to 60% of methadone is excreted unchanged. With prolonged use of the drug, its half—life varies widely – from 13 to 47 hours. Delayed clearance and the presence of a cumulative effect are due to the binding of methadone to plasma proteins and body tissues.
Indications
For detoxification in the treatment of opiate addiction (heroin addiction and dependence on other morphine-like drugs), as well as for the supportive treatment of patients with opiate addiction;
pain syndrome: moderate to severe, not relieved by non-narcotic analgesics (for tablets of 5 mg, 10 mg).
Contraindications
Hypersensitivity to methadone hydrochloride or to any other component of the drug;
respiratory depression (in the absence of necessary intensive care equipment);
the period of exacerbation of bronchial asthma;
accumulation of excess carbon dioxide in the blood;
diarrhea associated with pseudomembranous colitis caused by cephalosporins, lincomycin, clindamycin, penicillins;
diarrhea caused by poisoning;
intestinal obstruction;
simultaneous use with monoamine oxidase (MAO) inhibitors, as well as within 2 weeks after their withdrawal;
increased intracranial pressure, head injuries.
Methadone-3H is contraindicated for people who are addicted to “light” narcotic drugs (for example, codeine, pethidine and similar opiate receptor agonists).
Interactions with other drugs and other types of interactions
Opiate antagonists, mixed agonists/antagonists, partial agonists. Patients with heroin addiction or patients receiving supportive methadone therapy may experience withdrawal symptoms when taking opiate antagonists or drugs related to mixed agonists/antagonists. At least 20 hours should elapse between the use of buprenorphine and methadone.
Antihypertensive agents, in particular clonidine, prazosin, reserpine and urapidil, can enhance the effect of methadone.
Histamine H2 receptor antagonists, such as cimetidine, can reduce the level of a protein that binds to methadone, resulting in increased levels of opiates in the blood.
Anti-retroviral drugs. Nevirapine can reduce the concentration of Methadone-3H by increasing the metabolism of the latter in the liver. With the simultaneous use of Methadone-3H and nevirapine, the development of withdrawal syndrome was observed. If nevirapine is intended for patients receiving Methadone-3H, careful monitoring is necessary to detect withdrawal syndrome, and if necessary, the dose of Methadone-3H should be adjusted.
The simultaneous use of efavirenz and Methadone-3H in HIV-infected patients leads to a decrease in the concentration of Methadone-3H in blood plasma and the appearance of signs of withdrawal syndrome. It may be necessary to increase the dose of Methadone-3H.
When ritonavir and ritonavir / lopinavir are used simultaneously with Methadone-3H, there is a decrease in the concentration of Methadone-3H in blood plasma, although withdrawal syndrome is not always observed. However, the use of these drugs in combination with Methadone-3H requires caution.
The use of Methadone-3H leads to an increase in the area under the concentration-time curve (AUC) for zidovudine, which can lead to toxic effects.
The use of Methadone-3H leads to a decrease in AUC for didanosine and stavudine, for didanosine this effect is more pronounced. At the same time, the distribution of Methadone-3H does not change significantly.
Drugs that induce the converting enzymes of the cytochrome P450 system. The use of rifampicin in patients who have achieved stabilization with maintenance therapy with Methadone-3H leads to a significant decrease in the content of Methadone-3H in the blood serum when signs of withdrawal syndrome appear.
Taking phenytoin (250 mg 2 times a day on the first day, and then 300 mg 1 time a day for 3-4 days) by patients who underwent methadone therapy leads to a decrease in the concentration of Methadone-3H and the development of withdrawal syndrome. These phenomena disappear after the withdrawal of phenytoin. The pharmacokinetic parameters of Methadone-3H after withdrawal of phenytoin almost completely return to the initial level.
The administration of methadone together with other CYP3A4 inducers (e.g. St. John’s wort, phenobarbital, carbamazepine) may lead to withdrawal symptoms.
Cytochrome P450 inhibitors. The use of drugs that inhibit the activity of cytochrome P450 isoenzyme 3A4 may lead to a decrease in the clearance of Methadone-3H. As a result, there is an increase or prolongation of the effects of opiates. When prescribing drugs that are inhibitors of the isoenzyme, such as antifungal agents (including ketoconazole), macrolide antibiotics (including erythromycin), it may be necessary to adjust the dose of Methadone-3H. The use of certain selective serotonin reuptake inhibitors (for example, sertraline, fluvoxamine) together with Methadone-3H can lead to an increase in the content of Methadone-3H in blood plasma and to the appearance of toxic phenomena.
Repeated oral administration of voriconazole leads to an increase in the maximum plasma concentration and AUC for the pharmacologically active enantiomer of Methadone-3H (R-methadone) in patients receiving maintenance doses of Methadone-3H (30-100 mg 1 time per day). An increase in the concentration of Methadone-3H in blood plasma can lead to the development of toxic phenomena associated with an increase in the duration of the QT interval. It may also be necessary to reduce the dose of Methadone-3H.
Other drugs. The use of meperidine in therapeutic doses by patients who have been taking or have been taking MAO inhibitors for the last 14 days may lead to severe adverse reactions. Although such reactions have not been described for Methadone-3H, if it is necessary to use Methadone-3H in patients taking MAO inhibitors, it is necessary to make a sensitivity test, in which small doses are given to patients for several hours, gradually increasing them and registering the patient’s condition. The use of MAO inhibitors should be discontinued at least 14 days before the start of substitution therapy. Otherwise, it can lead to the development of a life-threatening depressing or stimulating effect on the central nervous system, respiration and blood circulation.
Protease inhibitors. The use of Methadone-3H together with agenerase (amprenavir) leads to a decrease in the maximum plasma concentration (Cmax) and AUC for R-methadone by 25% and 13%, respectively. With the simultaneous use of Methadone-3H and agenerase (amprenavir), careful monitoring of patients is necessary to prevent a decrease in the actual dose of Methadone-3H, especially if ritonavir is also used. The use of Methadone-3H and agenerase (amprenavir) leads to a decrease in AUC, Cmax and minimum plasma concentrations (Cmin) for agenerase (amprenavir) by 30%, 27% and 25%, respectively.
With the simultaneous use of viracept (nelfinavir) with Methadone-3H, changes in the content of Methadone-3H in blood plasma were noted. It may be necessary to increase the dose of Methadone-3H.
Non-nucleoside reverse transcriptase inhibitors. With the simultaneous use of Methadone-3H with a rescriptor (delavirdine), it may be necessary to reduce the dose of Methadone-3H.
Desipramine. When used simultaneously with Methadone-3H, the content of desipramine in blood plasma increases.
Potentially arrhythmogenic agents. Special care should be taken when using agents that can increase the duration of the QT interval, when combined with Methadone-3H. Such agents can be antiarrhythmic drugs of classes I and III, some neuroleptics and tricyclic antidepressants, calcium channel blockers. Caution should also be exercised when using drugs that disrupt the electrolyte balance in combination with Methadone, which can also contribute to prolongation of the QT interval (hypomagnesemia, hypokalemia). Such agents include diuretics, laxatives, and occasionally mineralocorticoids.
Interaction with other agents suppressing the activity of the central nervous system. Methadone-3H should be used with caution in patients who are prescribed other narcotic analgesics, general anesthesia, phenothiazines, other tranquilizers, sedatives and hypnotics, tricyclic antidepressants and other drugs that suppress the activity of the central nervous system, including alcohol, since such a combination can lead to respiratory depression, arterial hypotension, deep sedation and even a coma.
Interaction with serotonergic drugs. Serotonergic syndrome may occur when methadone is used concomitantly with pethidine, monoamine oxidase inhibitors (MAO) and serotonergic drugs such as selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitor (IOSSiN) and tricyclic antidepressants. Symptoms of serotonergic syndrome may include changes in mental state, autonomic instability, neuromuscular disorders and/or gastrointestinal symptoms.
Application features
If, after discontinuation of the drug, it is necessary to restore its intake again, then the initial dose should be low, it should be increased slowly to avoid serious toxic phenomena and respiratory depression.
Methadone-3H is intended for oral use only. The drug should not be used for injection.
When using Methadone-3H, morphine-type dependence may develop. Repeated use of Methadone-3H can lead to psychological and physical dependence, as well as to the development of tolerance. Therefore, the same caution should be exercised when using Methadone-3H as when using morphine.
If you suddenly switch from other opiates to Methadone-3H, there is a significant risk of respiratory depression, therefore, the transition to the use of Methadone-3H should be carried out with caution.
Incomplete cross-tolerance between methadone and other opiates. With tolerance to other opiates, partial tolerance to Methadone-3H is possible, especially in patients sensitive to other agonists of the m-opiate receptors. In the case of such tolerance, it is difficult to determine the dose of Methadone-3H. There are known fatal cases when switching to Methadone-3H after prolonged use of other opiate antagonists.
A high degree of opiate tolerance does not eliminate the question of the possibility of toxic phenomena when using Methadone-3H.
Interaction with alcohol and drugs. Methadone-3H has an additive effect when used simultaneously with alcohol, other opiate drugs, and has a depressive effect on the central nervous system. There are known fatal cases of the use of Methadone-3H by persons abusing benzodiazepines.
Anxiety states. Since Methadone-3H, which was used by people with tolerance to it in constant maintenance doses, is not a tranquilizer, patients receiving maintenance therapy using Methadone-3H develop anxiety states in response to stress and life problems. The doctor should not confuse these symptoms with withdrawal symptoms and should not try to treat such conditions by increasing the dose of Methadone-3H. The effect of Methadone-3H during maintenance therapy is limited to the control of opiate symptoms and does not extend to the relief of anxiety.
Head injuries and increased intracranial pressure. In head injuries, respiratory depression and increased cerebrospinal fluid pressure, which can be caused by Methadone-3H, turn out to be much stronger. The same danger exists in the case of other intracranial pathologies or with increased intracranial pressure, which was observed in patients earlier. The side effects of opiates can mask the real clinical condition of patients with head injuries.
Bronchial asthma and other respiratory disorders. The main danger with the use of Methadone-3H is the possible suppression of breathing. This problem is of particular importance for elderly patients, in weakened individuals, as well as in hypoxia or hypercapnia, when even moderate therapeutic doses can significantly reduce pulmonary ventilation.
Therefore, Methadone-3H should be prescribed with extreme caution in conditions accompanied by hypoxia, hypercapnia or reduced respiratory reserve, such as bronchial asthma, chronic obstructive pulmonary diseases, severe overweight, sleep apnea syndrome, myxedema, kyphoscoliosis, central nervous system depression, and coma. In these patients, even conventional therapeutic doses of Methadone-3H can cause depression of the respiratory center while increasing airway resistance, which can lead to respiratory arrest. In such cases, it is recommended to use non-opiate analgesics, and in case of their insufficient effectiveness, the use of Methadone is possible only with proper supervision of the patient.
Hypotensive effect. The use of Methadone-3H can lead to severe arterial hypotension in individuals who have impaired ability to maintain blood pressure due to a decrease in blood volume or with the simultaneous use of drugs such as phenothiazines or certain anesthetics.
Outpatient use. The use of Methadone-3H can disrupt mental and physical ability, the ability to work with sources of increased danger (driving a car, working with equipment). Methadone-3H, like other opioids, can cause orthostatic hypotension in outpatient patients.
Use for acute pain. In the case of physical injury, postoperative pain, or other cases of acute pain in patients receiving maintenance doses of Methadone-3H, these small doses will not be effective for analgesia. In such cases, it is necessary to prescribe analgesics, including opiates, indicated to relieve similar pain in other patients. Since Methadone-3H induces tolerance to opiates, higher doses of these drugs may be required.
The risk of relapse in drug addicts who receive maintenance therapy with methadone. Sudden discontinuation of opiates can lead to the development of withdrawal syndrome. At the same time, there is a risk of a return to independent drug use by the patient, it should be borne in mind when assessing the risk/benefit ratio when prescribing maintenance methadone therapy.
Tolerance and physical dependence. Tolerance is manifested in the fact that in order to maintain a certain effect, for example, analgesic, increasing doses of opiates are needed. Physical dependence manifests itself in the form of withdrawal syndrome after sudden discontinuation of the drug or when using its antagonist. Both tolerance and physical dependence can occur with long-term opioid therapy.
With the sudden cessation of Methadone-3H therapy, physically dependent patients may develop withdrawal syndrome. Both withdrawal syndrome and withdrawal syndrome are characterized by the following signs: anxiety, increased lacrimation, rhinorrhea, excessive sweating, feeling cold, yawning, myalgia, mydriasis. Other symptoms may develop: irritability, back pain, joint pain, weakness, stomach cramps, insomnia, nausea, anorexia, vomiting, diarrhea, increased blood pressure, increased heart rate, increased respiratory rate.
Usually, with prolonged use of Methadone-3H, sudden discontinuation of the drug is not recommended.
Features of application to patients of certain categories. Some categories of patients with Methadone-3H should be prescribed with caution and at a low initial dose (elderly patients, weakened patients, patients with severe liver or kidney dysfunction, hypothyroidism, Addison’s disease, prostatic hypertrophy, urethral strictures). It should also be borne in mind that the use of Methadone-3H can lead to respiratory depression.
Methadone-3H should be prescribed primarily to those patients in whom the benefits of opiate analgesia outweigh the known risk associated with the use of this drug (impaired cardiac conduction, respiratory depression, changes in mental status, postural hypotension).
Use in persons with impaired liver function. There is insufficient data on the use of Methadone-3H in persons with impaired liver function, however, it should be borne in mind that Methadone-3H is metabolized in the liver. Therefore, with impaired liver function, there is a risk of accumulation of Methadone-3H.
The effect on cardiac conduction. Methadone-3H is an inhibitor of the potassium channels of the heart and prolongs the QT interval. When using Methadone-3H, cases of serious arrhythmia (flickering and fluttering of the ventricles) were noted. Most often, these cases were noted with the use of high doses of Methadone-3H (more than 200 mg per day). In most cases, such complications occurred with repeated use of high daily doses to relieve pain, although there are cases where complications have developed with the use of maintenance therapy for opiate-dependent individuals.
In cases of an increased risk of prolongation of the QT interval, Methadone-3H should be used with caution (with cardiac hypertrophy, with simultaneous use of diuretics, with hypokalemia and hypomagnesemia). The use of Methadone-3H in patients with a history of conduction disorders or with a risk of rhythm disturbance is possible only with careful monitoring of the condition of such patients. In some cases, an increase in the duration of the QT interval with the use of Methadone-3H was also noted in patients with a history of cardiac dysfunction, especially when using high doses of the drug. With an increase in the duration of the QT interval during the use of Methadone-3H, it is necessary to try to eliminate known risk factors, in particular, pay attention to concomitant drugs that can affect cardiac activity, drugs that can change the electrolyte balance, as well as drugs that can inhibit the metabolism of Methadone-3H. When prescribing Methadone-3H for pain relief, it is necessary to take into account the risk of prolongation of the QT interval and cardiac arrhythmia. Such a risk should be compared with the possible benefits of treatment to eliminate the pain syndrome, and also take into account the availability of alternative therapies.
Methadone-3H treatment for analgesia in acute or chronic pain should be started only if the potential beneficial analgesic or palliative effect exceeds the risk of life-threatening complications possible with high doses of this drug.
When using Methadone-3H, an individual approach is necessary in comparing the possible benefits of treatment and the potential risk, taking into account both the medical history and the data of the clinical examination of the patient. When identifying risk factors, careful monitoring of the status of the cardiovascular system is necessary, including analysis of the duration of the QT interval and the occurrence of arrhythmias.
Adrenal insufficiency. Opioid analgesics can cause reverse adrenal insufficiency, which requires monitoring and replacement therapy with glucocorticoids. Symptoms of adrenal insufficiency may include, in particular, nausea, vomiting, loss of appetite, fatigue, weakness, dizziness or low blood pressure.
A decrease in the level of sex hormones and an increase in prolactin levels. Long-term use of opioid analgesics may be associated with a decrease in sex hormone levels and an increase in prolactin levels. Symptoms include decreased libido, impotence, or amenorrhea.
Hypoglycemia. Hypoglycemia is observed with an overdose or an increase in the dose of methadone.
Regular monitoring of blood glucose levels is recommended when increasing the dose (see sections “Overdose” and “Adverse reactions”).
Auxiliary substances. Due to the lactose content, the drug should not be taken in patients with rare hereditary galactose intolerance, Lapp lactase deficiency or glucose-galactose malabsorption syndrome.
If the patient is found to be intolerant of certain sugars, it is necessary to consult a doctor before taking this drug.
Method of administration and dosage
The drug is used only in specialized institutions. Patients taking the drug should be under close medical supervision and receive appropriate psychological and social support.
The initial dose for short-term detoxification
The dose is selected taking into account the individual clinical picture and subjective well-being of each patient, depending on the intensity of withdrawal symptoms. The general principle is to gradually adjust the dose to establish a minimum sufficient maintenance dose.
At the beginning of therapy, the average daily dose is 20 mg of methadone hydrochloride for patients with an undetermined or unknown threshold of drug dependence and 40 mg of methadone hydrochloride for patients with a known threshold of drug dependence and a long period of drug use. In exceptional cases, the initial daily dose can be increased to 100 mg.
The patient should take the first dose in the morning. In some cases, to prevent withdrawal syndrome, it is possible to prescribe an additional amount of the drug in the evening of the first day. In any case, the dose should always be sufficient to ensure that the symptoms of withdrawal syndrome do not exceed an acceptable level.
In the presence of such symptoms, the dose should be gradually increased by 10-20 mg. The maximum daily dose for adults is 120 mg per day.
Patients need to remember that the drug acts for a long time, as methadone accumulates in the tissues.
Changing the type of therapy
When transferring a patient from levomethadone to methadone hydrochloride, the dose calculation is carried out taking into account the ratio of 1: 2 (levomethadone: methadone hydrochloride), that is, 5 mg of levomethadone corresponds to 10 mg of methadone hydrochloride in effectiveness. In some cases, such a replacement may require additional dose adjustment of the latter.
Supportive therapy
During maintenance treatment, the drug should be titrated to a dose at which opiate symptoms do not appear for 24 hours, the need for a narcotic drug decreases, the euphoric effects of opiates are blocked or weakened, as well as when the patient is not sensitive to the sedative effect of methadone. In most cases, clinical stability is achieved at a daily dose of 80-120 mg.
Discontinuation of therapy after a period of supportive treatment
The cancellation of substitution therapy should be carried out slowly, with a gradual decrease in the daily dose over several weeks or months. There are significant differences in the methadone dose reduction regimens for patients who have chosen to discontinue methadone therapy under control. In general, it is confirmed that the dose should be reduced by less than 10% of the established maintenance dose, the dose should be reduced after 10-14 days. The patient should be informed about the high risk of drug dependence after discontinuation of maintenance treatment with methadone.
Pain syndrome
The dose of the drug should be carefully selected depending on the severity of pain and the patient’s reaction to the drug. It is safer to start treatment and titration of the methadone dose with a small initial dose with gradual dose adjustment.
Usually, methadone should not be used to relieve severe pain in patients who have not taken other opiate drugs.
Usually, adults are prescribed orally at a dose of 2.5–10 mg every 4 hours for the first 3-5 days, the dose is slowly titrated until the appropriate effect is achieved, then a fixed dose is applied every 8-12 hours, depending on the patient’s condition and his responses to treatment.
Elderly patients should use the drug 1 time per day.
To apply a dose of 2.5 mg, methadone hydrochloride should be prescribed in dosage form at an appropriate dose.
Method of application and duration of therapy
Tablets should be taken with a sufficient amount of liquid (1 cup of water).
The patient should be informed that oral administration of the drug is the only effective and safe way to use it.
The duration of therapy depends on the success of substitution therapy and the patient’s subjective well-being, taking into account the general principles of substitution therapy. The purpose of therapy is the patient’s refusal to use narcotic drugs. The duration of therapy can range from a short-term course (for example, as a substitute for narcotic substances for the period of stay of a drug-dependent person in a hospital) to long-term therapy.
The abolition of heroin.
At the beginning of substitution therapy, withdrawal symptoms are often observed, such as anxiety, anorexia, spontaneous convulsive obsessive movements, “goose bumps”, depression, diarrhea, vomiting, fever, yawning, weight loss, nausea, sneezing, pupil dilation, irritability, rhinorrhea, physical pain, dizziness, increased lacrimation, excessive sweating, intestinal cramps, tachycardia, tremor, restlessness, stomach cramps, involuntary muscle twitching, change of chills to hot flashes. The frequency and severity of side effects gradually decrease over several weeks.
The initial dose.
Special attention should be paid to the individual selection of the initial dose. Too high doses in the initial period can cause side effects.
The most dangerous side effects when using methadone are respiratory depression and hypotension.
Deaths have been reported.
Side effects such as dizziness, sedation, nausea, vomiting, and increased sweating are most often observed. In such cases, you can reduce the dose of methadone.
Use in persons with impaired liver function.
With prolonged maintenance methadone therapy, there is a gradual decrease in side effects over several weeks, although side effects such as increased sweating and constipation remain.
With prolonged maintenance methadone therapy, there is a gradual decrease in side effects over several weeks, although side effects such as increased sweating and constipation remain.
Other adverse reactions that are recorded when using methadone
From the blood side: bleeding, reversible thrombocytopenia, eosinophilia.
From the side of the psyche: euphoria, a state of depression, hallucinations, dysphoria, convulsive seizures.
From the nervous system: drowsiness, sedation, confusion, fainting, disorientation, headache, fatigue, insomnia, agitation.
From the organ of vision: visual impairment (dysopia).
From the cardiovascular system: palpitations, bradycardia, edema, arterial and orthostatic hypotension, cardiac arrest, circulatory disorders, shock, inversion of the T wave, arrhythmia, extrasystole, fluttering and flickering/ventricular fibrillation, prolongation of the QT interval, bigeminia, syncope, cardiomyopathy, heart failure, phlebitis.
From the respiratory system: respiratory depression, respiratory arrest, pulmonary edema, worsening of the course of bronchial asthma.
From the digestive tract: nausea, vomiting, dry mouth, constipation, abdominal pain, anorexia, glossitis.
From the side of the hepatobiliary system: biliary tract spasm.
From the skin and subcutaneous tissues: excessive sweating, urticaria, skin rash, itching, redness, hot flashes.
From the genitourinary system: delayed and impaired urination, amenorrhea, decreased libido and/or potency.
Others: hypokalemia, hypomagnesemia, hypoglycemia, decrease or increase in body weight, asthenia, weakness, development of tolerance.
Methadone-3H is an agonist of the m-receptors of opiates, therefore, when using the drug, dependence of the same type may develop as when using morphine.